Home / Sleep apnoea
What is sleep apnoea?
What are the characteristics of sleep apnoea syndrome?
Sleep apnoea is characterised by repeated involuntary respiratory arrest while sleeping. An apnoea occurs if air flow is stopped for a minimum of 10 seconds but this can go on for more than one minute. Doctors also refer to hypopnoea, which is a reduction in air flow to the lungs of at least 30%, resulting in a drop of at least 4% in the oxygen level in the blood.
There are two types of sleep apnoea:
- Obstructive sleep apnoea syndrome (OSAS) is the most common case. This type of apnoea is due to a relaxation of the tongue and the throat muscles which relax and collapse on the airways. The air passage is thus completely blocked.
- Central sleep apnoea is caused by a dysfunction in the brain that no longer sends the command to breathe.
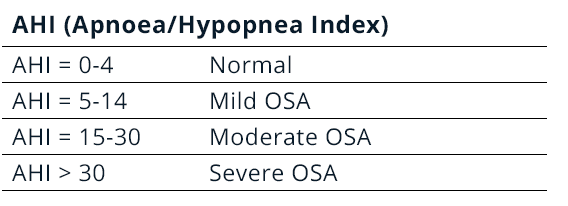
Apnoea is considered pathological if you stop breathing more than 5 times per hour. Beyond 15 times per hour we speak of moderate apnoea and beyond 30 times per hour is called severe apnoea.
Obstructive Sleep Apnoea Syndrome (OSAS) is also referred to if the rate of apnoea and hypopnoea (AHI) exceeds 5 per hour and is associated with symptoms such as drowsiness, sensations of suffocation or in the presence of associated cardiovascular pathologies.
Who is affected by sleep apnoea?
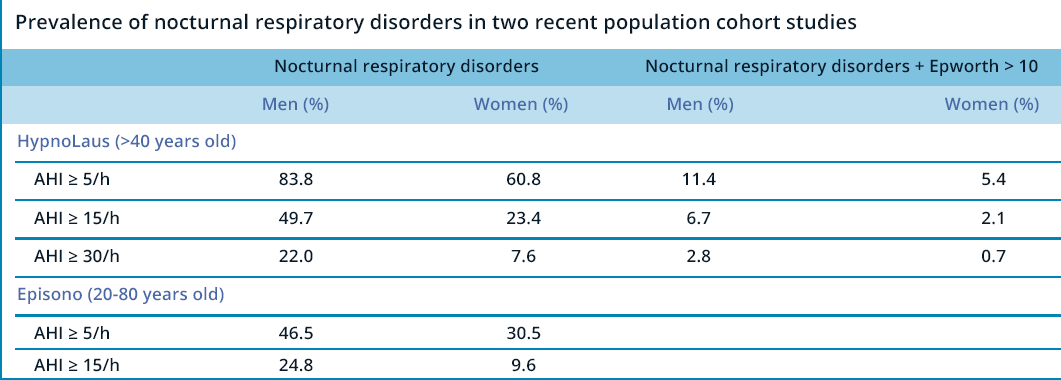
Sleep apnoea can affect anyone, whether you are a child, an adult, overweight or underweight. There are different estimates of the number of people affected by sleep apnoea. According to the most recent and large epidemiological study published on this pathology 1, sleep apnoea affects 49% of men and 23% of middle-aged to elderly women.
Who is affected by sleep apnoea?
During sleep, apnoea does not occur evenly but preferably in certain positions (on the back). Thus it is estimated that apnoea occur only in the dorsal position in 27% of apnoeic patients. Apnoea also occurs preferably in certain stages of sleep (REM).This is probably due to the fact that during this phase of sleep the muscles of the pharynx become more relaxed, which leads to airway obstruction, causing snoring and apnoea.
Being male, your age and obesity are the most important risk factors leading to nocturnal respiratory disorders. For example, the frequency of moderate apnoea (AHI>15/h) increases from 28% in 40–60-year-olds to 48% in 60–80-year-olds. This increase seems to be due to age-related loss of muscle tone and is particularly significant in women due to the menopause, which causes the pharyngeal tissues to sag. Obesity also has a significant impact with a frequency of sleep apnoea that is 2.8 times higher in overweight people (BMI > 30). Indeed, in the event of being overweight, the fatty tissues infiltrate the pharyngeal muscles more, which leads to a loss of tonicity causing them to sag and thus obstructing the airways.
Certain anatomical features also play an important role in the development of obstructive sleep apnoea. For example, retrognathia (recessed lower jaw) causes the tongue to move towards the pharynx. Also a bulky tongue (macroglossia), enlarged tonsils or a very long soft palate favour airway obstruction and the appearance of obstructive events that cause sleep apnoea and snoring.
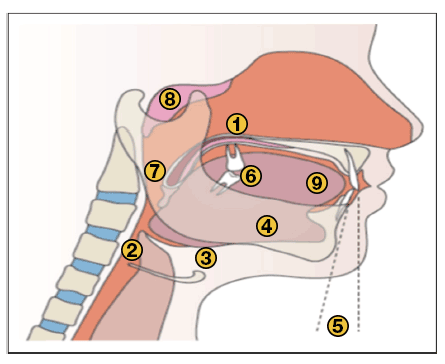
Upper airway abnormality described in patients with obstructive sleep apnoea syndrome. Modified based on Lévy and al. Nat Rev Dis Primers 2015 [1]
1: long and enlarged uvula; 2: reduced retropharyngeal space; 3: lowering of the hyoid bone; 4: verticalization of the mandible; 5: retro-position of the mandible; 6: loss of dental occlusion; 7: enlarged tonsils; 8: enlarged adenoids; 9: macroglossia.
In addition to these physiological factors, there are also exogenous factors such as alcohol, antidepressants or tobacco, which will favour the relaxation of tissues and increase the risk of obstruction of the air passage.
Say goodbye to snoring!
Oniris® oral device
- Unique comfort to sleep peacefully
- Unmatched clinical effectiveness
- Secure online payment
What are the consequences of this sleep disorder?
Obstructive sleep apnoea syndrome is a pathology that can have serious consequences. Repeated episodes of apnoea-hypopnoea lead to a drop in oxygen levels and sleep fragmentation, which activate numerous mechanisms (oxidative stress, tissue inflammation) causing serious cardiovascular and metabolic consequences.
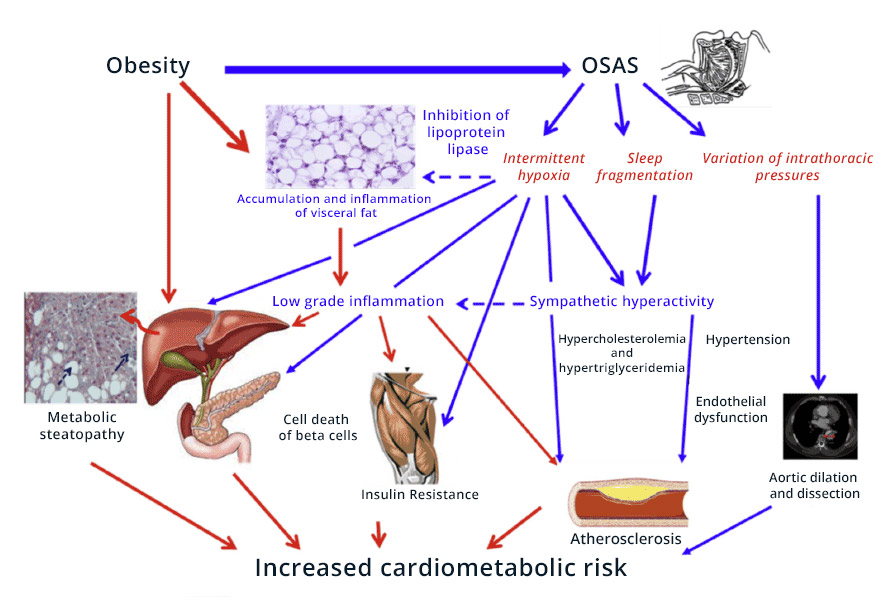
OSAS (obstructive sleep apnoea syndrome): pathophysiology of cardio-metabolic consequences. Modified based on Pépin and al. Thorax 2012 [24]
In adults, sleep apnoea is associated with several significant pathologies:
- Risk of high blood pressure multiplied by 5, and 40% of people with high blood pressure suffer from apnoea.
- Risk of coronary heart disease multiplied by 5.
- Risk of atrial fibrillation multiplied by 4.
- Risk of ventricular tachycardia multiplied by 3.
- Risk of stroke increased by 60%, and 60% of those affected suffer from sleep apnoea.
- Risk of Cancer multiplied by 4.8 in severe cases.
- Risk of type 2 diabetes, twice as frequent in snorers and 4 times more frequent in people with sleep apnoea.
- Risk of Alzheimer’s disease, which appears 10 years earlier in people who snore and suffer from sleep apnoea.
- Risk of depression multiplied by 1.6 to 2.6 depending on the severity of the apnoea.
- Risk of road and work accidents multiplied by 5 in the case of apnoea due to a drop in alertness linked to lack of sleep.
Beyond these consequences that can lead to premature death, there are also many disabling symptoms that affect the quality of physical, social and mental life:
- Fatigue and drowsiness
- Mood swings, depression
- Difficulty concentrating
- Memory problems
- Libido disorders
Sleep apnoea in children is also associated with learning and growth disorders.
All of this results in a high cost to the health of the untreated person suffering from sleep apnoea. In fact, the cost will be twice as high, as they have more hospitalisations, medical consultations and drug treatments.
This cost is also important because of the decline in productivity levels at work and the increase in accidents at work. For example, the American Academy of Sleep Medicine has estimated the cost of lost productivity in the US due to untreated sleep apnoea at $87 billion.
Despite its harmful impact, this sleep apnoea syndrome is too often overlooked, its symptoms appear mild or harmless and 75% of cases of sleep respiratory disorders go undiagnosed.
How to detect sleep apnoea?
Several signs and symptoms should alert and lead to a diagnostic examination.
During the day you should be concerned if you notice certain signs such as tiredness or drowsiness, mood changes, depression, difficulty concentrating or memory problems, and even a headache in the morning.
Other signs are more noticeable in the evening or at night, such as chronic snoring, suffocation, waking up with a feeling of suffocation, urinating several times a night, night sweats or libido problems.
Screening questionnaires can also help to identify a risk of sleep apnoea. Perhaps the most recognised by the medical community is the Berlin questionnaire and the STOP BANG test.
If several of these signs are present, it is imperative to make an appointment to diagnose sleep apnoea.
How is sleep apnoea diagnosed?
The diagnosis is a simple and painless operation. Simply make an appointment with a specialist. They may be ENT doctors, Respirologists, Cardiologists, General Practitioners, etc. The patient’s sleep will then be recorded in the laboratory or at home.
What are the recommended treatments for sleep apnoea?
There is a myriad of available treatments for snoring and sleep apnoea on the market and it is sometimes difficult to choose the right one. Unfortunately, many of them do not work and only a few of the proposed treatments have proven results and are recognised.
Treatments that really work
As we have seen, this is a serious pathology and in order to make a decision it is therefore better to refer to the opinion of the health authorities and the scientific community. In this case, the Health Authorities consider that only 2 alternatives are really effective and recommended as first-line treatments, continuous positive pressure and mandibular advancement devices:
| Clinical situation | First-line treatment | Second-line treatment |
|---|---|---|
| AHI > 30 | CPAP | MAD |
|
AHI = 15-30 With at least 10 micro-awakenings | CPAP | MAD |
|
AHI = 15-30 With cardiovascular comorbidities | CPAP | MAD |
|
AHI = 15-30 Without associated severity sign (Less than 10 micro-awakenings per hour, no cardiovascular comorbidities) | MAD | / |
Mandibular advancement devices (MADs) reduce sleep apnoea and its symptoms such as subjective daytime drowsiness or sleeping disorders at night. They improve quality of life, reduce blood pressure and are recommended in the treatment of patients suffering from mild to moderate obstructive sleep apnoea.
Mandibular advancement devices can be custom moulded by dentists, but this is relatively expensive (over £1,000), time consuming and only 5% of dentists are trained to make them.
However, there is a solution: Oniris mandibular advancement devices. On sale over the counter for about £99and available in several sizes, they can be completely personalised as they are dipped in boiling water to be able to take customised impressions. Studies have shown that they perform just as well as custom-made oral devices.
Other brands of oral devices that are immersed in hot water also exist but have not been subject to clinical studies. Their results are therefore generally poorer and they can lead to more uncomfortable side effects or even a significant risk in the long term. They are therefore generally not recommended.
The Continuous Positive AirwayPressure (CPAP) device allows you to breathe pressurised air into a mask, which clears the airways.
Although very effective, the Continuous Positive Pressure Device is very expensive and restrictive during the night, which leads many patients to abandon the treatment in the long term.
Treatments that can be used in certain cases
In case of failure of these 2 treatments and in some particular cases, other solutions can be proposed.
Surgery of the soft palate or tonsils is possible, but only in case of hypertrophy of these tissues.
Intranasal corticosteroids improve mild to moderate OSAS in children with concomitant rhinitis and/or upper airway obstruction due to endocapillary hypertrophy.
A positional treatment to avoid sleeping on your back. According to the European Respiratory Society, it can lead to a moderate reduction in the apnoea-hypopnoea index (younger, less active and less obese patients), but it is significantly lower than CPAP and MAD and therefore cannot be recommended except in carefully selected patients. This solution is reserved for patients who spend most of their time on their back when sleeping, which concerns less than one in four people. Long-term compliance with positional treatment is poor.
Solutions to avoid
Other solutions should be avoided.
Pharmacological treatments are not recommended and should be avoided such as benzodiazepines, opioids and sildenafil.
Nasal devices come in 2 types. Nasal dilators that increase the opening of the nostrils. According to the European Respiratory Society they are not recommended to reduce snoring or improve breathing disorders or sleep architecture. Nasal tubes for intubation through the nose are not recommended by health authorities and learned societies for the treatment of snoring or sleep apnoea. There is insufficient data to judge their value and the act of nasal intubation can lead to serious consequences such as persistent bleeding, inflammatory and allergic reactions, as well as purulence. Intubation also increases the risk of infection, sinusitis or pneumonia.
Sources:
- Epidémiologie, population à risque et phénotypes cliniques du syndrome d’apnées du sommeil. [Epidemiology, population at risk and clinical phenotypes of sleep apnoea syndrome.] La Presse Medicale, 46 (2017) 388-394. doi:10.1016/j.lpm.2016.11.002
- Physiopathologie du syndrome d’apnées-hypopnées obstructives du sommeil et de ses conséquences cardio-métaboliques. [Physiopathology of the obstructive sleep apnoea-hypopnoea syndrome and its cardio-metabolic consequences.] La Presse Medicale, 46 (2017) 395-403. doi:10.1016/j.lpm.2016.09.008
- Sleep-disordered Breathing and Cancer Mortality, Results from the Wisconsin Sleep Cohort Study. Am J Respir Crit Care Med Vol 186, Iss. 2, pp 190-194, Jul 15, 2012
- Impaired glucose-insulin metabolism in males with obstructive sleep apnoea syndrome Eur Respir J 2003; 22: 156–160
- Sleepiness-Related Accidents in Sleep Apnea Patients. SLEEP, Vol. 23, No. 3, 2000
- https://aasm.org/resources/pdf/sleep-apnea-economic-crisis.pdf
- Young et al. Sleep Disordered Breathing and Mortality. Eighteen-year follow-up of the Wisconsin Sleep Cohort. Sleep 2008; 31(8):1071-1078
- French National Authority for Health. Évaluation clinique et économique des dispositifs médicaux et prestations associées pour la prise en charge du syndrome d’apnées hypopnées obstructives du sommeil (SAHOS). [Clinical and economic evaluation of medical devices and associated services for the management of obstructive sleep apnoea hypopnoea syndrome (OSAHS).] Part 1: Volet médico-technique et évaluation clinique. [Medical-technical component and clinicalevaluation.] July 2014.
- French National Authority for Health. Fiche de bon usage des technologies de santé. [Healthtechnology instructions for use sheet.] Comment prescrire les dispositifs médicaux de traitement du syndrome d’apnées hypopnées obstructives du sommeil chez l’adulte. [How to prescribe medical devices for the treatment of obstructive sleep apnoea syndrome in adults.] October 2014.
- Randerath*et al. The European Respiratory Society task force on non-CPAP therapies in sleep apnoea. Eur Respir J 2011; 37: 1000–1028
- -G. Brivet. Intubation nasotrachéale : le débat. [Nasotracheal intubation: the debate.] Réanimation (2014) 23:6-8 [Resuscitation (2014) 23:6-8]
ONIRIS – Class I medical device manufactured by ONIRIS SAS and indicated in the treatment of snoring and sleep apnoea – Read the leaflet carefully before use – Ask your doctor or pharmacist for advice. This medical device is a regulated health product which, under these regulations, bears the CE mark.
Say goodbye to snoring!
Oniris® oral device
- Unique comfort to sleep peacefully
- Unmatched clinical effectiveness
- Secure online payment
A complete range of oral devices to meet your needs
| ONIRIS | ONIRIS Pro | Tali | |
|---|---|---|---|
| Freedom of movement | |||
| Millimetre-adjustment of the advancement | |||
| Custom-made impression | |||
| Clinically approved for snoring | |||
| Clinically approved for sleep apnoea | |||
| Approved by the French National Authority for Health | |||
| Developed by a trained dentist | |||
| Custom-made | |||
| Waiting time | 24-48 hours | 30 days | 3 to 9 months |
| Average lifespan | 12 to 24 months | 12 to 24 months | 5 years |